Diagnosing and Managing Hormonally Associated Migraine
Fredrick Freitag, DO
Migraines and Menses
Slide 1. Diagnosing and Managing Hormonally Associated Migraine
This discussion will address specific management issues on menstrually
associated migraine: why it is important to recognize it, and what we can do
optimize management in women who struggle with the chronic condition that
presents with acute episodes of disabling attacks.
Slide 2. Definitions
True menstrual migraine is a headache that occurs in women who primarily
have migraine during menses. The "menstrual window" is often defined
as 2 days before the onset of the menstrual flow, to 1 or 2 days after the
onset of flow. Many women, however, have menstrually associated migraine.
The drop in estrogen associated with menses is a trigger factor for
migraine in susceptible women. Other migraine sufferers also are susceptible
to other endogenous factors, such as the onset of menarche, pregnancy, and
menopause. Exogenous factors include oral contraceptives and use of hormone
replacement therapy.
What do we know about menstrually associated migraine, and why do we have
an interest in this process? For some patients, menstrually associated
migraine may be different in its response to therapies or treatment strategies
as compared with migraine that occurs outside the menstrual window.
Slide 3. Menstrual Cycle and Headache in a Population Sample of
Migraineurs
One study by Stewart evaluated women who had migraine and other headache
types. Specific headache types were assessed in relationship to presence of
menses over a 1-month period.
Slide 4. Headaches and Menstrual Cycle
Stewart and colleagues reported that women who had migraine with aura --
where they have the well-defined visual phenomena preceding the attack by 20
to 30 minutes or so -- really showed very little difference over the course of
the month in attack frequency in relation to hormone fluctuations. However,
those with migraine without aura had an increase in headache frequency during
the menstrual window. This study also reported that women who had tension-type
headache have the same kind of phenomena.
One reason for the increase in frequency of tension-type headache that
occurred during the menstrual window is that these participants might have
been misdiagnosed, and they were actually migraine sufferers who thought they
had tension-type or sinus headache. Additionally, some patients have 1 or 2
diagnostic criteria for migraine, but fail to meet all the criteria -- we
sometimes consider these to be "migrainous headaches."
Slide 5. A View of Migraine and Menstrual Associated Migraine (MAM)
Menstrually associated migraine is a genetically determined process. If you
do not have migraine headache, you do not have a sensitized trigeminal system,
and the hormonal changes don't trigger the attack. However, migraine sufferers
appear to have a sensitive brain that includes a sensitive trigeminal system.
Hormonal fluctuations, specifically estrogen, serve as a triggering factor for
eliciting the attack by altering the threshold that is required for activation
of the migraine process.
Diagnosing and Managing Hormonally Associated Migraine
Fredrick Freitag, DO
Estrogen Levels and Migraine Headaches
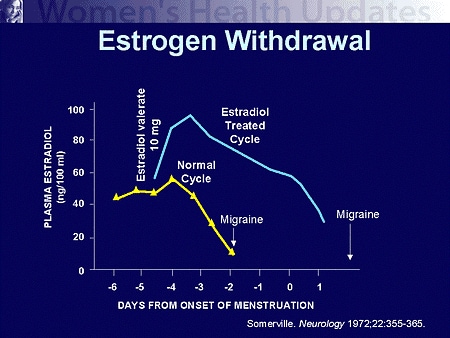
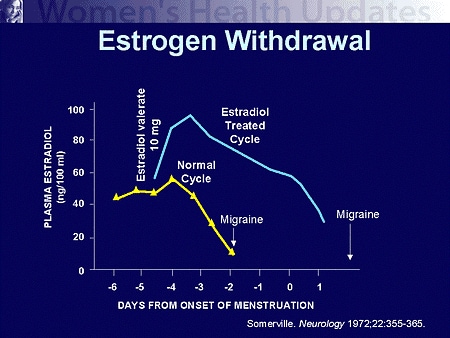
Slide 6. Estrogen Withdrawal
How do we know that declining estrogen levels are the precipitating factor
for onset of an attack in susceptible women? We are relying on a single study
done in 1972 by Somerville in Australia. He looked at a group of women who
reported menstrual migraine and put them through a series of challenges, using
either estrogen or progesterone. The progesterone challenge did not alter the
tendency for the migraine to occur, but it did have an effect on the tendency
for when menses did begin.
However, when Somerville challenged these women with a depot dose of an
estrogen compound, we see that the estrogen levels change, and with it, as the
estrogen levels now fall off much later because of the role of the depot
estrogen, the headache occurs later.
Slide 7. Migraines Coincide With E2 Falls
Clinically, we know that estradiol levels change in relationship to the
menses. Estradiol drops 1 to 2 days before the onset of the menses. Although
less pronounced, there also is a decrease in estradiol during ovulation.
Similarly, when women go onto the placebo days while on oral contraceptives,
estradiol decreases. In the old days, when I trained, we routinely cycled
women on and off of their hormone replacement therapy. Taking them off their
estrogen product for the last 10 days of their cycle would trigger their
migraine attacks.
Because there is going to be some variability in estrogen levels even with
the patches and with the depot injections, as we get toward the end of the
therapeutic range of those treatments, the decreasing estrogen levels may also
be responsible, in part, for triggering migraine attacks.
Additional evidence for estrogen as a factor comes from endogenous triggers
associated with pregnancy and delivery. After delivery, there is a marked
decrease in estradiol concentrations, which in some women is followed by
postpartum headache or migraine.
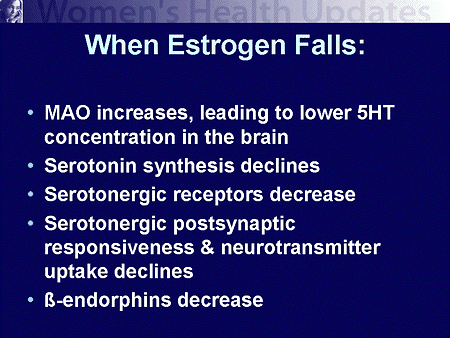
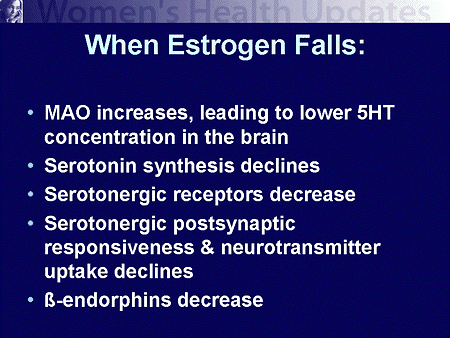
Slide 8. When Estrogen Falls
Women will often ask me, "What's wrong with my hormones that I'm
getting these headaches?" There's nothing wrong with their hormones.
Their hormones are behaving normally if they are having normal menstrual
periods. But it is the change in hormones that elicits a variety of other
physiological changes that actually precipitate and trigger this whole process
of migraine.
One of the things that happens is that there is a change in concentration
of the enzyme monoamine oxidase (MAO). MAO is the enzyme found in the gut and
in the brain that metabolizes serotonin, which we know to be a very important
neurotransmitter substance in the migraine process. This change in MAO enzyme
causes a fall in serotonin levels to occur, again, setting that threshold up
for transition into the migraine process.
In response to decreasing estrogen levels, there may be a change in the
neural junctions with the receptors for serotonin. There is a decrease in the
number of receptor sites. Postsynaptically, we see alterations in response in
this reuptake of serotonin occurring because of the change in estradiol
levels. Additionally, we also see a change in endorphins, the brain's natural
painkillers. The brain becomes physically sensitized to pain because of this
decrease in the endorphins related to the declining estrogen levels.
Slide 9. Summary: Sex Hormones and Migraine
In summary, migraine is a process that occurs in women more commonly than
men, and goes through a natural history of change and effect over a woman's
lifetime. During youth, boys are a little more likely to get migraine headache
than girls. But with the onset of puberty (menarche), we see this epidemiology
of the disorder change. After puberty, there is a higher preponderance of
migraine in women. By the time we get into the middle years of life, women
outnumber men with migraine by a 3:1 ratio.
Along with this, because of the effects of the estrogen changes that occur
cyclically each month, we see a tendency for migraine to occur more commonly
around the time of the menses. Some women who get migraine only have migraine
at their menses. This is a relatively rare phenomenon, and is often referred
to as "true menstrual migraine". The majority of women have hormonal
factors playing a triggering role in their overall tendency to have an attack,
and they will have attacks both inside and outside the menstrual window.
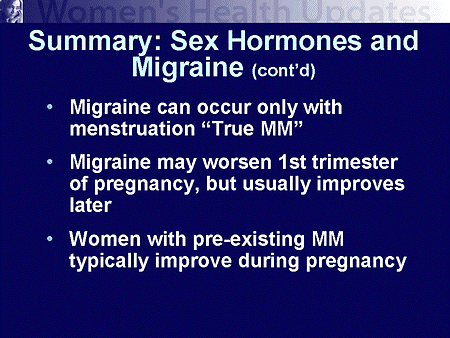
Slide 10. Summary: Sex Hormones and Migraine (cont'd)
A good number of women who have migraine headache have a period of
remission that occurs during the last 2 trimesters of pregnancy. Part of the
reason for this relates to the fluctuating estrogen levels during the first
trimester. During the second and third trimester, estradiol levels are quite
high and relatively stable. It is this stability in the estrogen levels that
helps to induce the remission during the last 2 trimesters of pregnancy.
Slide 11. Summary: Sex Hormones and Migraine (cont'd)
During the adult reproductive years, women are exposed to hormone
replacements in a variety of forms and fashions. Oral contraceptives and
hormone replacement therapy can have effects, both good and bad, on the
occurrence of their migraine attacks. Some women have an ablation of their
migraines by taking oral contraceptives or by going on hormone replacement
therapy on a steady basis in the menopausal years. Other women have a
worsening of the attacks. If that occurs, it may be a signal to use an
alternative compound to see if that makes a difference in the occurrence of
the attacks. It is also a red flag for women who have significant changes
neurologically with their migraine attacks with the start of use of an oral
contraceptive or hormone replacement therapy, because these are the women who
may have higher risk for complications of their migraines, such as stroke,
occurring.
Thankfully, getting old does have some benefits when it comes to migraine.
One of the few benefits of aging is that migraine subsides as women get older,
especially as they move into their menopausal years. There is a flattening of
the estradiol changes, whether because they occur naturally or because of
hormone replacement therapy, and they are maintained at a set level. So we
need to be sensitive to these factors in the life cycle of women and their
migraine headaches.
Diagnosing and Managing Hormonally Associated Migraine
Fredrick Freitag, DO
Management of Menstrual Migraine Headaches
Slide 12. Management of Migraine Associated With Menses
Let us look at some of the aspects of management of migraine associated
with menses.
Slide 13. Pharmacotherapy of Migraine Associated With Menses (MAM)
There are several different approaches that we can take. We can use acute
therapeutics that treat the attack as it occurs, and we can use prevention to
try to ameliorate propensity for the headaches from occurring at all around
the menstrual period. We will look at acute treatment first.
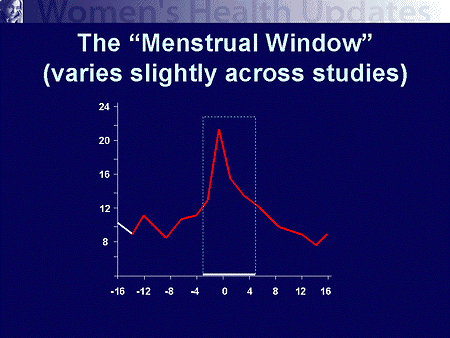
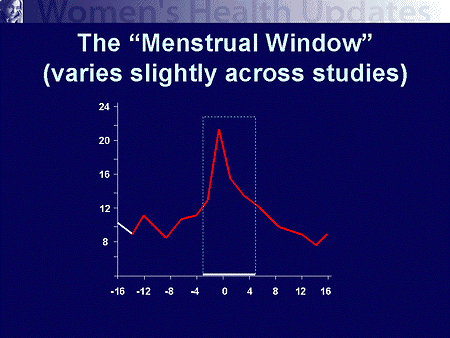
Slide 14. The "Menstrual Window" (Varies Slightly Across
Studies)
One of the challenges we face when studying and identifying menstrual
migraine is defining the disorder. When is it a menstrually associated
migraine attack? Based upon the clinical trial and research that is involved,
there is a window that exists, from as much as 3 days before the onset of flow
to as long as 5 days after the onset of flow, as being that potential
menstrually associated migraine treatment window, with variability between the
studies.
Diagnosing and Managing Hormonally Associated Migraine
Fredrick Freitag, DO
Sumatriptan and Menstrual Migraine Headaches
Slide 15. Prospective Study in MAM: Sumatriptan 6 mg SC
The first of the studies that looked at menstrually associated migraine
involved the injectable form of sumatriptan: a 6 mg subcutaneous dose. This
was done by Facchinetti from Italy.
This group looked at the occurrence of menstrually associated migraine and
its response to the injection of subcutaneous sumatriptan in a
placebo-controlled trial. In this trial they had the women treat 2 migraine
attacks during the menstrual window. They then looked at both 1-hour as well
as 2-hour time points following the injection. Within 1 hour of treating the
attack with subcutaneous sumatriptan, there was an approximately 70% response
rate of reduction in headache response (decrease in pain intensity from
moderate or severe to mild or none). This was quite significant vs placebo. By
2 hours, we had further improvement, approaching the 80% level of women who
had a positive response with their menstrually associated migraine. Again,
highly significant results vs placebo.
Slide 16. Retrospective Study With Sumatriptan 6 mg SC in MAM
A second study was done by Solbach. This was a retrospective study: they
gathered chart data and looked at the response of subcutaneous sumatriptan in
treating menstrually associated migraine. As in the previous study, there was
a statistically significant improvement in achieving a headache response over
placebo. Nausea, vomiting, and light sensitivity were markedly reduced as part
of that response to the sumatriptan compared with the placebo group, which
still maintained 80% of the women having photophobia 1 hour into the attack.
Slide 17. Oral Sumatriptan in MAM
One of the challenges with sumatriptan 6 mg subcutaneous is the injectable
delivery. There are several different oral triptans and even nasal sprays that
may prove helpful in menstrual migraine.
There are several studies to date on oral tablets, the first of which was
with sumatriptan in the oral formulation. This study used the highest dose
available, 100 mg.
Trial designs for migraine headache, in general, call for patients to begin
treatment once the headache pain becomes moderate to severe, which is the
current standard practice for clinical studies, not clinical practice.
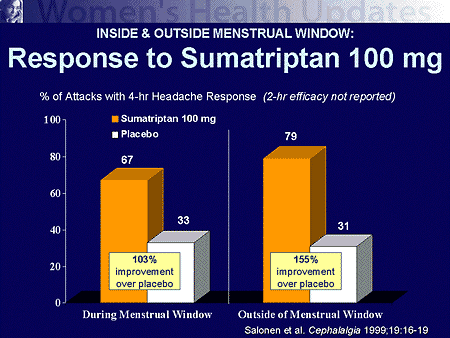
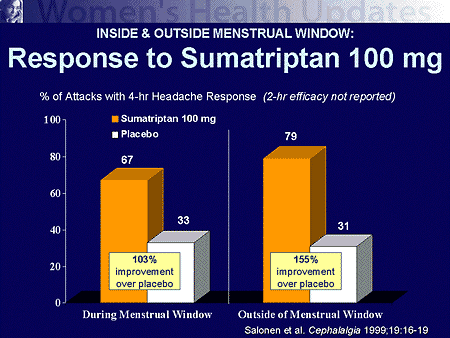
Slide 18. Inside & Outside Menstrual Window: Response to
Sumatriptan 100 mg
The first of these studies looked at attacks, not only menstrually
associated, but also nonmenstrually associated. The authors report that there
was a significant difference over placebo in achieving a headache response. It
was not a huge difference, but if you look at the attacks of migraine that
occurred during this menstrual window, by comparison with those attacks
treated outside the menstrual window, there was a little over 10% difference
in response rates between the 2 time frames for these individuals, and very
little difference in the placebo arm of this study. It does suggest that there
may be a difference in response, and that menstrual migraine requires a
slightly different therapeutic approach from nonmenstrually associated
migraine.
Diagnosing and Managing Hormonally Associated Migraine
Fredrick Freitag, DO
Rizatriptan and Menstrual Migraine Headaches
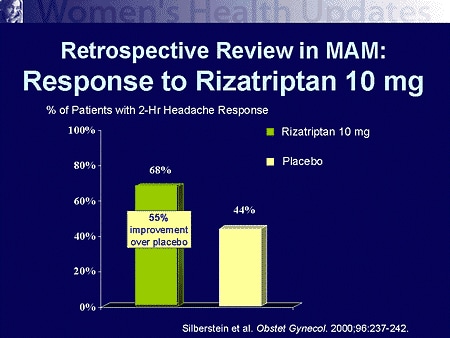
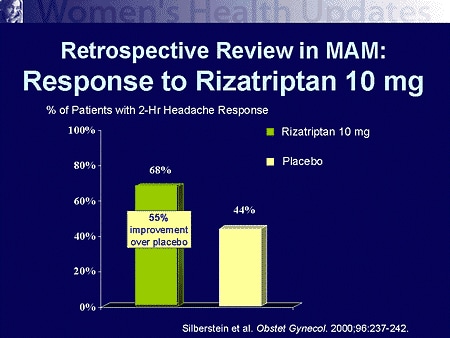
Slide 19. Retrospective Review in MAM: Response to Rizatriptan 10 mg
Similar results were shown in a retrospective study with rizatriptan oral
tablets. This study looked at time frame related to menses, by days in the
period as well as when the attack was treated. Overall, there was a 68%
response rate in the rizatriptan group, and approximately a 44% placebo
response rate.
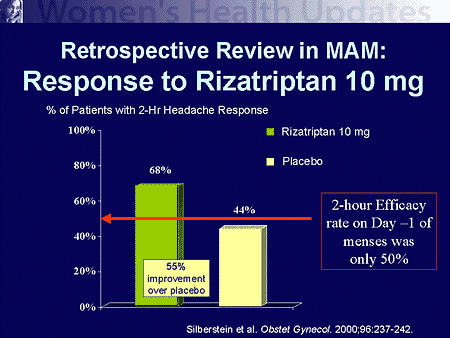
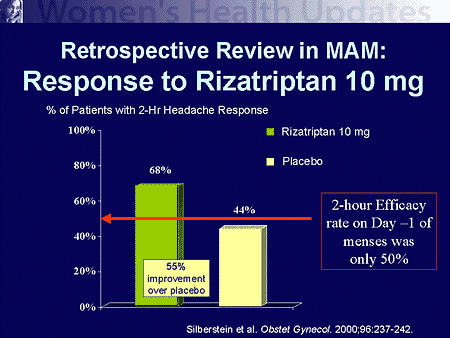
Slide 20. Retrospective Review in MAM: Response to Rizatriptan 10 mg
If we look at when in this menstrual window the migraine attack was treated
with rizatriptan, on day -1 of the cycle, the day before onset of flow, the
response rate was only 50%, compared with almost 70% for the entire window.
This suggests that day -1 of menses is associated with a lower headache
response rate, which coincides with the highest drop in estrogen levels.
Diagnosing and Managing Hormonally Associated Migraine
Fredrick Freitag, DO
Zolmitriptan and Menstrual Migraine Headaches
Slide 21. Retrospective Meta-analysis in MAM: Response to
Zolmitriptan
To evaluate the efficacy of zolmitriptan, there have been 2 studies
reported in the literature to date. One study was retrospective and one was
prospective. The retrospective study performed a meta-analysis utilizing the
data from all of the controlled clinical trials that led up to the
registration and approval of the drug. There has certainly been some
controversy in the headache field about how good meta-analyses are, but they
certainly do serve a role. They are a standard, statistical method for looking
at treatment across a variety of clinical trials.
In looking at the data retrospectively from the registration and other
trials for zolmitriptan, they found that there was very little difference in
response rate of those migraine attacks that were treated associated with the
menses in this 3- to 5-day window compared with those attacks that were
treated outside of the menstrual window. There was a little bit of favor for
the 5 mg dose over the 2.5 mg dose when the attacks were inside the menstrual
window.
Slide 22. Zolmitriptan in Migraine Associated With Menses (MAM)
Retrospective studies help us look for trends and identify possible
clinical benefits, but, obviously, the best way to assess clinical evidence
for treatment efficacy is using prospective trials. A prospective,
double-blind, placebo-controlled trial with zolmitriptan was carried out
utilizing a range of potential dosages based upon the intensity of the
headaches. Patients used 1.25, 2.5, or 5 mg of zolmitriptan to treat migraine
of mild, moderate, and severe intensity, respectively.
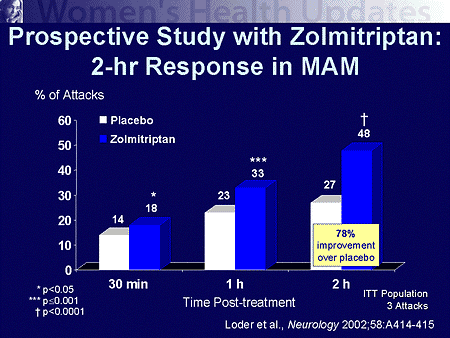
Slide 23. Prospective Study With Zolmitriptan: 2-hr Response in MAM
Remember, these data do not look at dosages specifically, but these women
were allowed to treat based upon their severity with the dose that they
thought most appropriate, from a small dose to a large dose. So they were able
to gauge what kind of treatment level they should have. But in this
prospective trial, we saw a very early response. About 18% of women had relief
for their migraine attack within the first 30 minutes of taking their dose of
oral zolmitriptan. And by 2 hours, it was about 48%. That is a little bit
lower than we would expect to see, in general, from the clinical trials, but
it was still highly significant compared with the placebo arm.
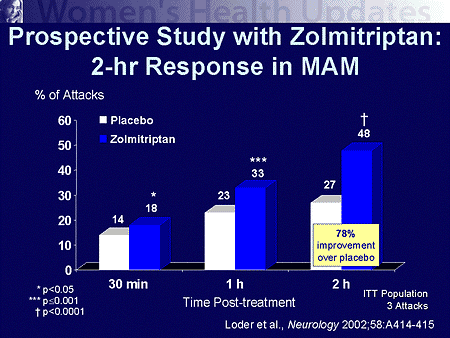
Slide 24. Prospective Study With Zolmitriptan: 2-hr Response in MAM
This improvement over placebo was observed at 1 and 2 hours as well.
Diagnosing and Managing Hormonally Associated Migraine
Fredrick Freitag, DO
Analgesia and Menstrual Migraine Headaches
Slide 25. Pharmacotherapy of Migraine Associated With Menses
We have seen that the acute treatment is reasonably effective, and not far
off the mark compared with the treatment of migraine outside of the menstrual
window. Still, this is a problematic disorder if the attacks do not respond
well to treatment. Therefore, we sometimes want to turn toward the preventive
approach to block propensity for the attacks to occur. Several different
approaches can be used along this line.
Slide 26. Naproxen Mini Prophylaxis
Probably the most common approach that we utilize for prevention of
menstrually associated migraine is the use of nonsteroidal anti-inflammatory
drugs taken on a mini-preventive basis, where we begin the nonsteroidal
several days before the woman expects her menstrually associated migraine
attack to occur. This has been looked at in a controlled clinical trial using
naproxen sodium, a 550 mg dose, twice daily.
Treatment was begun about a week before the onset of the expected menstrual
flow and was continued into the sixth day following the onset of flow. They
did a series of treatments during successive months to evaluate the response,
and it was a placebo-controlled trial.
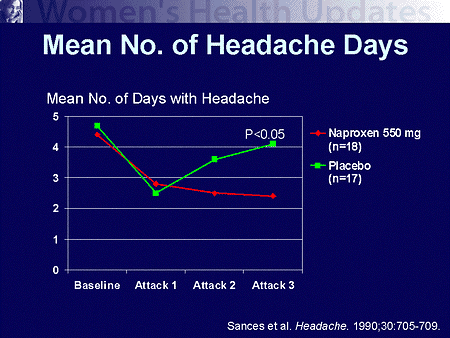
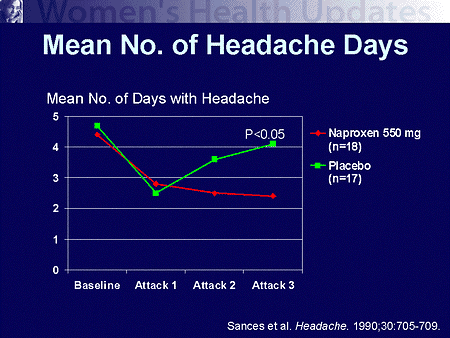
Slide 27. Mean No. of Headache Days
This demonstrates one of the problems in doing placebo-controlled trials.
If we look at a single window of opportunity, we see that in that first
therapeutic month, the placebo worked as well as the active therapy -- a
little disconcerting. However, with treatment over the subsequent 2 menstrual
cycles, we see what would normally be expected in a placebo-controlled trial
-- there is a regression of the placebo response back toward the mean. We also
see that clear statistical difference occurring where there is a substantial
reduction in the number of days of menstrually associated migraine occurring
with the use of a nonsteroidal. Instead of having 4 days of headache,
menstrually associated in a cycle, women taking the naproxen sodium 550 mg in
the second and third months had about 2 days of attack. That is a nice
reduction.
Slide 28. Analgesic Use
One thing that was also looked at was the effect on the use of additional
medications, analgesic requirements for treating these menstrually associated
migraines.
When we looked at the untreated phase there was, unfortunately, a
difference between the active and placebo groups, but women in the active
group required on average 4 doses of an analgesic medication per day during
the menstrually associated window. With the use of the naproxen sodium, we had
a drop-off to a little over 1 dose per day that was needed. So we had a very
marked reduction. Again, there was an early placebo response with first cycle,
but the typical regression to the mean with treating multiple attacks. One of
the issues we must monitor closely is presence of gastrointestinal side
effects when patients are using nonsteroidal anti-inflammatory drugs. Also,
patients should be closely monitored for overuse (defined for many as using
acute medications more than 2 to 3 days per week).
Diagnosing and Managing Hormonally Associated Migraine
Fredrick Freitag, DO
Naratriptan and Menstrual Migraine Headaches
Slide 29. Naratriptan "Mini Prophylaxis"
Using the science of nonsteroidals, what other approaches can we utilize to
prevent menstrually associated migraine? One of the techniques that has become
of interest and has been utilized fairly widely is to use these triptan
medications, which we use acutely, as a mini-preventive approach for
menstrually associated migraine. A study done using naratriptan for this
purpose used 1 mg vs 2.5 mg, the standard dose, vs the placebo. They treated
in the menstrual window of an approximately 5-day period of time and they
treated over a series of cycles.
Slide 30. Naratriptan "Mini Prophylaxis"
Unfortunately, in this study we saw some very unusual results. First of
all, the 2.5 mg dose was no more effective than placebo. Not an expected
result when you are using a medication. Additionally, the lower dose was
effective to reduce the number of menstrually associated migraines by
approximately 50%. This was statistically significant.
However, given the cost of triptan medications and the number of attacks
that were involved, the cost averaged over $300 per "headache to
avoid" with this kind of treatment. It was a very expensive therapeutic
when you compare it with the cost of naproxen sodium. So, we need to look at
cost-effectiveness of these kinds of approaches for prevention of migraine as
well.
Diagnosing and Managing Hormonally Associated Migraine
Fredrick Freitag, DO
Hormonal Manipulation and Menstrual Migraine Headaches
Slide 31. Hormonal Manipulation
A third approach that we utilize is hormone manipulation. This is certainly
a very adequate approach for some as well.
Slide 32. Hormonal Manipulation Goals
The goal here is to change that paradigm of the drop in estradiol. We can
do so by adding a supplement of estrogen perimenstrually, reducing the total
falloff and keeping the other levels more constant.
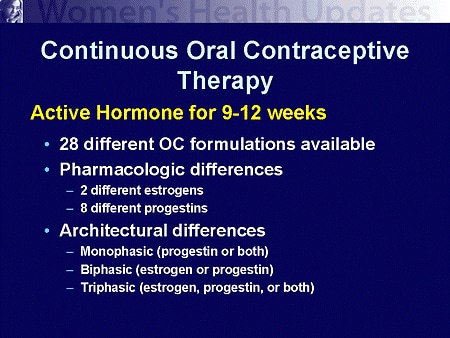
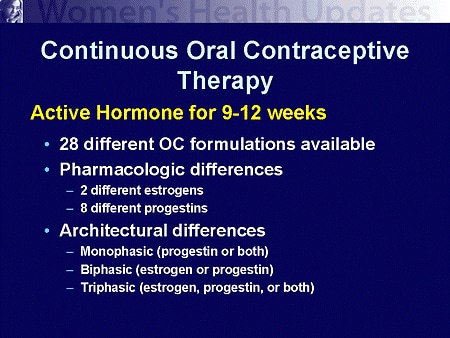
Slide 33. Continuous Oral Contraceptive Therapy
We can even use oral contraceptives to do this, where we have the woman
utilize the active pill packs over a series of cycles with no days off from
the active therapeutic. There are different methods of doing that with
different hormonal oral contraceptive compounds. This is certainly broad --
there are over 28 formulations available that we could utilize. This is a very
effective method for many women who have very severe menstrual migraine.
Commonly we will have a woman cycle for 3 months on the pill before taking
a cycle off. Instead of having 12 menstrually associated migraine periods a
year, you now have 4, which can make a remarkable difference for many women.
In Europe, the standard may be as long as a year between having menstrual
flows by taking a cycle off the pill. It is really the standard of care for
your practice that makes a difference here.
Diagnosing and Managing Hormonally Associated Migraine
Fredrick Freitag, DO
Summary
Slide 34. Summary
In summary, the menses is a common trigger for migraine headache, because
of the changes in estrogen and estradiol levels associated with normal
menstrual cycles. The changes in the estrogen levels that do occur with
supplemental estrogen use may again have an influencing effect for the good
and therefore we all need to be sensitive to these issues.
When it comes to treating menstrually associated migraine it may be a
little more challenging a disorder to treat than migraine outside of the
menses, but we do know that the triptans are very effective for acute
treatment of this process and can be utilized as first-line therapy.
Prospective studies have specifically supported this for sumatriptan and
zolmitriptan. The nonsteroidal approach is certainly a very cost-effective
one, and did cause a substantial reduction in the number of attacks that were
treated (caution for gastrointestinal adverse events and overuse).
For those women who may not be candidates for triptans or chose not to use
acute treatments, hormonal manipulation may help bring better control and
better quality of life to those women who have difficult migraine associated
with their menses, especially if they are on oral contraceptive or hormone
replacement therapy already.
Faculty and Disclosures
Authors
Fredrick Freitag, DO
Clinical Associate Director, Department of Family Medicine,
Finch University Health Sciences/Chicago Medical School;
Associate Director, Diamond Headache Center, Chicago, Illinois
Disclosure: Dr. Freitag has conducted research for and/or served
on the speakers' bureau and/or served as a consultant for Abbott
Laboratories, Allergan, AstraZeneca, Bayer Pharmaceuticals,
Brisol-Myers Squibb Co, CAPNIA, Elan Pharmaceutical, Epicept,
GlaxoSmithKline, Janssen Pharmaceuticals, Merck & Co., Inc.,
Novartis, Pfizer, Inc., Pharmacia, Pozen, Winston, and Wyeth
Ayerst Laboratories.
|
|