Cardiology
-
Acute coronary Sx

STEMI
-
"MONA F HABS"
Troponin levels may also be elevated in:
-
CHF
cardiomyopathy
cardiac contusion
myocarditis
pericarditis
renal insufficiency
PE
severe infections
shock
certain chronic inflammatory conditions of muscles and skin.
-
Morphine sulfate 2-4 mg IV
with increments of 2-8 mg IV repeated at 5-15 min intervals.
-
Supplemental O2 during 1st 6 hrs.
If SaO2 < 90% or overt pulmonary congestion → O2 continued beyond 1st 6 hrs.
-
If ongoing ischemic discomfort → NTG 0.4 mg SL q 5 mins x 3
If persistent ischemia, CHF, or Htn → NTG IV.
If recurrent angina or persistent CHF > 48 hrs after STEMI → NTG IV, PO, or topical.
In view of their marginal treatment benefits, nitrates should not be used if hypotension limits the administration of beta-blockers, which have more powerful salutary effects.
Contraindications:
-
systolic <90 mm Hg
systolic > 30 mm Hg below baseline
severe bradycardia (<50 bpm)
tachycardia (>100 bpm)
suspected RV infarction
phosphodiesterase inhibitor within 24 hrs (48 hrs for tadalafil)
ASA
- ASA 162-325 mg PO chewed
-
Fibrinolytic therapy should be administered if:
-
symptom onset w/n 12-24 hrs who have continuing ischemic symptoms and
ST elevation > 0.1 mV in
-
≥ 2 contiguous precordial leads or
≥ 2 adjacent limb leads
or with new (or presumably new) LBBB
-
Absolute contraindications:
-
● Asymptomatic patients whose initial symptoms began > 24 hrs earlier
● only ST-segment depression (except if a true posterior MI is suspected)
● Any prior ICH
● Known structural cerebral vascular lesion (e.g. AVM)
● Known malignant intracranial neoplasm (primary or metastatic)
● Ischemic stroke < 3 mos EXCEPT acute ischemic stroke within 3 hrs
● Suspected aortic dissection
● Active bleeding or bleeding diathesis (excluding menses)
● Significant closed head or facial trauma < 3 mos
Relative contraindications:
-
● H/o chronic, severe, poorly controlled Htn
● sBP > 180 or dBP > 110
● H/o prior ischemic stroke > 3 mos, dementia, or known intracranial pathology not covered in absolute contraindications
● Traumatic or > 10 mins CPR
● Major surgery < 3 wks
● Within 2-4 wks internal bleeding
● Noncompressible vascular punctures
● For streptokinase/anistreplase: prior exposure > 5 days ago or prior allergic reaction
● Pregnancy
● Active peptic ulcer
● Current use of anticoagulants
Unfractionated heparin
-
UFH 60 U/kg (maximum 4000 U) bolus
followed by an initial infusion of 12 U/kg/hr (max 1000 U/hr)
adjusted to maintain aPTT 1.5-2.0 x control (approx 50-70 s).
LMWH
-
LMWH might be considered an acceptable alternative
to UFH if:
-
< 75 y/o & Cr > 2.5 mg/dL in men or 2.0 mg/dL
in women
Enoxaparin 30 mg IV bolus
followed by 1.0 mg/kg sc q12h
until hospital discharge used in combination
with full-dose tenecteplase
DVT prophylaxis with sc LMWH or with sc UFH 7,500-12,500 U BID until completely ambulatory, may be useful.
-
Target INR 2-3 for >3 months if:
-
Persistent atrial fibrillation
Extensive wall motion abnormalities
Severe LV systolic dysfunction
LV thrombus
Previous systemic or pulmonary embolism
Immediate β-blocker therapy appears to reduce the magnitude of infarction, the risk of reinfarction, and the risk of life-threatening ventricular tachyarrhythmias.
Contraindications:
-
β-blockers or calcium channel blockers should not
be administered acutely to STEMI patients with frank
cardiac failure evidenced by pulmonary congestion or
signs of a low-output state.
β-blockers should be initiated before discharge for secondary prevention. For those who remain in heart failure throughout the hospitalization, low doses should be initiated, with gradual titration on an outpatient basis.
-
ACEI PO within 1st 24 hrs of STEMI to patients with anterior infarction, pulmonary congestion, or LVEF < 40%
if no hypotension (systolic < 100 or > 30 below baseline).
IV ACE inhibitor should not be given b/c risk of hypotension.
E.g. captopril 1.0 - 6.25 mg PO TID
Valsartan (target: 160 mg BID) should be administered to STEMI patients who are intolerant of ACEI.
Diuretic
-
Low- to intermediate-dose furosemide if pulmonary congestion with associated
volume overload. Caution is advised for patients who have not received volume expansion.
-
If LVEF < 40% and either symptomatic CHF or DM
& already receiving therapeutic doses of ACEI →
L-T aldosterone blockade
if Cr > 2.5 mg/dL in men & > 2.0 mg/dL in women &
K+ < 5.0
Non-DHP CCB
-
If ongoing ischemia or atrial fibrillation or flutter with rapid ventricular
response →
may give verapamil or diltiazem when β-blockers are ineffective or contraindicated
contraindications: CHF, LV dysfunction, AV block.
-
It is reasonable to use anxiolytics to alleviate short-term anxiety or altered behavior related to hospitalization.
-
DHP CCBs
Nifedipine (immediate-release form) is contraindicated b/c risk of hypotension → reflex tachycardia.
Estrogen plus progestin
-
should not be given de novo to postmenopausal women after
STEMI for secondary prevention of coronary events.
Postmenopausal women who are already taking estrogen plus progestin at the time of a STEMI should not continue hormone therapy.
Thiazolidinediones
-
should not be used in patients
recovering from STEMI who have NYHA class III or IV CHF.
-
Patients with STEMI who are free of recurrent ischemic
discomfort, symptoms of heart failure, or serious
disturbances of heart rhythm should not be on bed rest
for more than 12-24 hours.
After 12-24 hours, it is reasonable to allow patients with hemodynamic instability or continued ischemia to have bedside commode privileges.
Diagnostic coronary angiography should be performed in candidates:
-
for PCI
with cardiogenic shock who are candidates for revascularization
for surgical repair of ventricular septal rupture or severe mitral regurgitation
with persistent hemodynamic and/or electrical instability
with failed reperfusion (eg, recurrence of chest pain and persistence of ECG findings indicating infarction)
mechanical complications (eg, sudden onset of heart failure or presence of a new murmur)
Pulmonary edema + hypotension = Dx: cardiogenic shock
A preshock state of hypoperfusion with normal blood
pressure may develop before circulatory collapse and is
manifested by cold extremities, cyanosis, oliguria, or decreased
mentation.
→ If BP permits, afterload-reducing agents → ↓ cardiac
work & pulmonary congestion
→ dobutamine infusion
→ IABP → improved coronary perfusion & ↓ afterload → ↓ cardiac work
→ PCI or CABG (Early revascularization is reasonable for selected patients who develop shock w/n 36 hrs)
of MI
1. Oxygen supplementation to SaO2 >90%
2. Morphine
3. Titration of short-acting ACEI
4. Possible insertion of IABP for the management of refractory pulmonary congestion
The immediate management goals include adequate oxygenation and preload reduction to relieve pulmonary congestion. Because of sympathetic stimulation, the blood pressure should be elevated in the presence of pulmonary edema. Patients with this appropriate response can typically tolerate the required medications, all of which lower blood pressure.
Inferior STEMI and hemodynamic compromise:
- should be assessed with a V4R lead & echocardiogram
to screen for RV infarction.
Inf STEMI → RV dysfunction → ↓ CO
Mgt: flds → ↑ RV preload → ↑ CO
Treatment of RV ischemia/infarction includes early maintenance of RV preload, reduction of RV afterload, inotropic support of the dysfunctional RV, early reperfusion, and maintenance of AV synchrony.
Patients with pulmonary congestion or hypotension often need inotropic and vasopressor agents and/or IABP.
IABP (intra-aortic balloon pump) counterpulsation
If:
-
STEMI & hypotension (systolic <90 mm Hg or 30 mm Hg below baseline mean arterial pressure) who do not respond to other interventions.
Rehabilitation
On the basis of assessment of risk, ideally with an
exercise test to guide the prescription, all patients
recovering from STEMI should be encouraged to
exercise for a minimum of 30 minutes, preferably daily
but at least 3 or 4 times per week (walking, jogging,
cycling, or other aerobic activity), supplemented by an
increase in daily lifestyle activities (eg, walking breaks
at work, gardening, and household work).
Cardiac rehabilitation/secondary prevention programs are recommended particularly for those with modifiable risk factors.
Treatment with cognitive-behavioral therapy and selective serotonin reuptake inhibitors can be useful for depression that occurs in the year after hospital discharge.
The patient?s list of current medications should be reevaluated in a follow-up visit, and appropriate titration of ACE inhibitors, beta-blockers, and statins should be undertaken.
The predischarge risk assessment and planned workup should be reviewed and continued. This should include a check of LV function and possibly Holter monitoring for those whose early post-STEMI ejection fraction was 30-40% or lower, in consideration of possible ICD use.
The psychosocial status of the patient should be evaluated in follow-up, including inquiries regarding symptoms of depression, anxiety, or sleep disorders and the social support environment.
If symptoms recur, patients should be advised to call 911 after 5 minutes despite possible feelings of uncertainty and fear of embarrassment.
NSTEMI
-
Diagnostic evaluation of suspected UA/NSTEMI
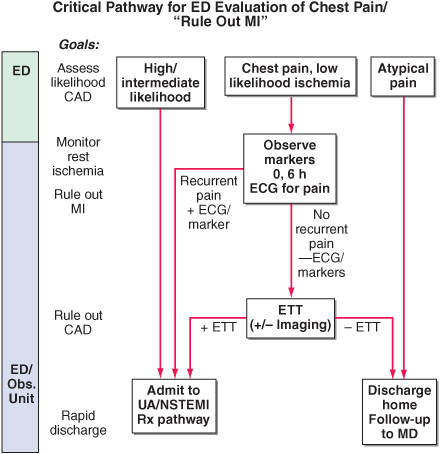
Patients with a low likelihood of ischemia are observed in a monitored bed over a period of 6 h, and 12-lead EKGs are performed if the patient has recurrent chest discomfort. A panel of cardiac markers (e.g., troponin and CK-MB) is drawn at baseline and 6 h later.
If the patient develops recurrent pain, has ST-segment or T-wave changes, or has positive cardiac markers → admit to hospital and treat for UA/NSTEMI.
If the patient has negative markers and no recurrence of pain, he/she is sent for exercise treadmill testing, with imaging (e.g. MIBI, stress echo) reserved for patients with abnormal baseline electrocardiograms (e.g. LBBB or LVH).
If low risk of embolization → low dose ASA long term + clopidogrel x 8-12 months.
Risk-stratification
Killip classification
| Killip class | Criteria | Mortality w/n 30 days |
| I | no clinical signs of heart failure | 6% |
| II | lung crackles, S3, elevated JVP | 17% |
| III | frank acute pulmonary edema | 38% |
| IV | cardiogenic shock or hypotension (sBP <90 mmHg), peripheral vasoconstriction (oliguria, cyanosis, or sweating) | 81% |
Unstable angina

Atherosclerosis
-
Risk factors
| Major | Constitutional | Minor
| DM
| age
| sedentary
| Htn
| sex
| obesity
| dyslipidemia
| FHx
| stress
| smoking
|
|
| |
Canadian Cardiovascular Society (CCS) Angina Grading Scale
| Class | Criteria |
| I | Angina only during strenuous or prolonged physical activity |
| II | Slight limitation, with angina only during vigorous physical activity |
| III | Symptoms with everyday living activities, i.e. moderate limitation |
| IV | Inability to perform any activity without angina or angina at rest, i.e. severe limitation |
Atrial fibrillation
CHAD2
(C for CHF, H for Htn, A for age, D for diabetes, and 2 for CVA/TIA which gets two points)
| CHF | 1 |
| systolic > 160 | 1 |
| ≥ 75 y/o | 1 |
| DM | 1 |
| Prior cerebral ischemia | 2 |

If score = 1 → ASA
If score ≥ 2 → warfarin → INR 2-3
CHF
New York Heart Association (NYHA) Functional Classification of Heart Failure
| NYHA Class | Symptoms |
|---|---|
| I | No symptoms and no limitation in ordinary physical activity |
| II | Mild symptoms (mild shortness of breath and/or angina) and slight limitation during ordinary activity. |
| III | Marked limitation in activity due to symptoms, even during less-than-ordinary activity, e.g. walking short distances (20-100 m). Comfortable only at rest. |
| IV | Severe limitations. Experiences symptoms even while at rest. Mostly bedbound patients. |


Valsartan (Diovan) 40 mg BID → target: 160 mg BID
Metoprolol 12.5 mg PO BID → ↑ by 50-100% q 2-4 wks to target of 100 mg PO BID
Furosemide 20-40 mg qd or BID (max 600 mg/d)
-
Framingham Cardiovascular Risk Calculator
U.K. Cardiovascular Risk Calculator
Risk reduction targets
| Risk group | 10-yr risk CVD | Target LDL | Target TC/HDL
| High
| >20%
| <2.0
| <4.0
| Moderate
| 10-20%
| <3.5
| <5.0
| Low
| <10%
| <5.0
| <6.0
| |
High risk automatically includes coronary artery disease, peripheral artery disease, cerebrovascular disease, and most patients with diabetes.
Hypertension
-
If average BP ≥ 140/90 on three occasions, Dx of Htn confirmed.
If diastolic BP > 130 or BP > 180/110 with signs/symptoms (papilloedema, retinal hemorrhage), then urgent treatment.
If average BP ≥ 160/100 or BP < 160/100 with DM, CKD, LVH or vascular dementia or CHD risk ≥ 20% over 10 years, then pharmacologic treatment with lifestyle management.
If not, then lifestyle management and reassess regularly. If lifestyle management insufficient (BP ≥ 140/90), then pharmacologic treatment.
INVESTIGATIONS:
-
Urinalysis
microalbuminuria (albumin/creatinine ratio)
blood chemistry (potassium, sodium, creatinine/eGFR)
FBG
lipids
ECG
Framingham risk assessment (10-year CHD risk) or UKPDS risk assessment if DM2
-
Mgt
Diastolic +/- systolic Htn:
- ACEI, ARB, BB, CCB, thiazide,
Isolated systolic Htn:
- ARB, LA DHP-CCB, thiazide
DM (esp. if ↑ACR):
- ACEI, ARB, furosemide (prn if Cr>150)
Angina:
- ACEI, ARB
MI:
- ACEI, ARB
Heart failure (NYHA III or IV):
- ACEI, ARB
LVH:
- ACEI, ARB, LA DHP-CCB, thiazide
Non-acute CVA or TIA:
- ACEI + thiazide combination
Non-diabetic CKD:
- ACEI, ARB
Syncope
-
Syncope DDx.ppt
Cardiovascular
- bradydysrhythmias
tachydysrhythmias
AS
IHSS
MI
HF
massive PE
subclavian steal Sx
Reflex mechanisms
- vasovagal
micturition
deglutition
cough
carotid sinus hypersensitivity
Orthostatic hypotension
- hypovolemia
drugs (e.g. antidepressants, antihypertensives)
dysautonomias
Psychogenic
-
hysterical
panic disorder
anxiety disorder
Unknown (18%)