|

Young and
Depressed
Ten years ago this
disease was for adults only. But as teen depression comes out of the
closet, it’s getting easier to spot—and sufferers can hope for a brighter
future
By Pat Wingert and Barbara
Kantrowitz
NEWSWEEK |
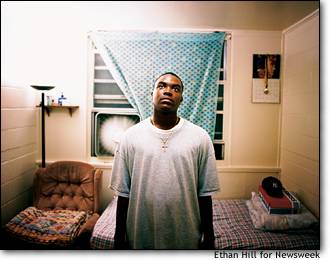
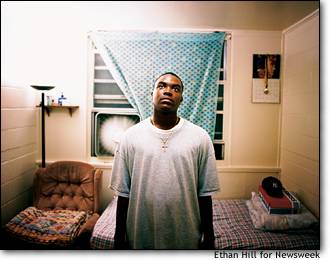
 Eric Suarez,
17, who suffers from bipolar disorder, takes nine medications daily to
treat his depression-some for the symptoms and others to combat the side
effects of those drugs. Eric Suarez,
17, who suffers from bipolar disorder, takes nine medications daily to
treat his depression-some for the symptoms and others to combat the side
effects of those drugs.
|
|
Oct. 7 issue —
Brianne Camilleri had it all:
two involved parents, a caring older brother and a comfortable home near
Boston. But that didn’t stop the overwhelming sense of hopelessness that
enveloped her in ninth grade. “It was like a cloud that followed me
everywhere,” she says. “I couldn’t get away from
it.”
 BRIANNE STARTED DRINKING and experimenting with drugs.
One Sunday she was caught shoplifting at a local store and her mother,
Linda, drove her home in what Brianne describes as a “piercing silence.”
With the clouds in her head so dark she believed she would never see light
again, Brianne went straight for the bathroom and swallowed every Tylenol
and Advil she could find—a total of 74 pills. She was only 14, and she
wanted to die.
BRIANNE STARTED DRINKING and experimenting with drugs.
One Sunday she was caught shoplifting at a local store and her mother,
Linda, drove her home in what Brianne describes as a “piercing silence.”
With the clouds in her head so dark she believed she would never see light
again, Brianne went straight for the bathroom and swallowed every Tylenol
and Advil she could find—a total of 74 pills. She was only 14, and she
wanted to die.
A few hours later Linda
Camilleri found her daughter vomiting all over the floor. Brianne was
rushed to the hospital, where she convinced a psychiatrist (and even
herself) that it had been a one-time impulse. The psychiatrist urged her
parents to keep the episode a secret to avoid any stigma. Brianne’s
father, Alan, shudders when he remembers that advice. “Mental illness is a
closet problem in this country, and it’s got to come out,” he says. With a
schizophrenic brother and a cousin who committed suicide, Alan thinks he
should have known better. Instead, Brianne’s cloud just got darker. After
another aborted suicide attempt a few months later, she finally ended up
at McLean Hospital in Belmont, Mass., one of the best mental-health
facilities in the country. Now, after three years of therapy and
antidepressant medication, Brianne, 19, thinks she’s on track. A sophomore
at James Madison University in Virginia, she’s on the dean’s list, has a
boyfriend and hopes to spend a semester in Australia—a plan that makes her
mother nervous, but also proud.
AN ‘EPIDEMIC’?
Brianne is one of the lucky ones. Most of the nearly 3 million
adolescents struggling with depression never get the help they need
because of prejudice about mental illness, inadequate mental-health
resources and widespread ignorance about how emotional problems can wreck
young lives. The National Institutes of Mental Health (NIMH) estimates
that 8 percent of adolescents and 2 percent of children (some as young as
4) have symptoms of depression. Scientists also say that early onset of
depression in children and teenagers has become increasingly common; some
even use the word “epidemic.” No one knows whether there are actually more
depressed kids today or just greater awareness of the problem, but some
researchers think that the stress of a high divorce rate, rising academic
expectations and social pressure may be pushing more kids over the
edge. |
|
Resources
|
|
|
How to get
help |
|
|
|
This is a huge change from a decade ago, when many doctors considered
depression strictly an adult disease. Teenage irritability and
rebelliousness was “just a phase” kids would outgrow. But scientists now
believe that if this behavior is chronic, it may signal serious problems.
New brain research is also beginning to explain why teenagers may be
particularly vulnerable to mood disorders. Psychiatrists who treat
adolescents say parents should seek help if they notice a troubling change
in eating, sleeping, grades or social life that lasts more than a few
weeks. And public awareness of the need for help does seem to be
increasing. One case in point: HBO’s hit series “The Sopranos.” In a
recent episode, college student Meadow Soprano saw a therapist who
recommended antidepressants to help her work through her feelings after
the murder of her former boyfriend.
Without
treatment, depressed adolescents are at high risk for school failure,
social isolation, promiscuity, “self-medication” with drugs or alcohol,
and suicide—now the third leading cause of death among 10- to
24-year-olds. “The earlier the onset, the more people tend to fall away
developmentally from their peers,” says Dr. David Brent, professor of
child psychiatry at the University of Pittsburgh. “If you become depressed
at 25, chances are you’ve already completed your education and you have
more resources and coping skills. If it happens at 11, there’s still a lot
you need to learn, and you may never learn it.” Early untreated depression
also increases a youngster’s chance of developing more severe depression
as an adult as well as bipolar disease and personality disorders.
|
|
NEW APPROACHES
For
kids who do get help, like Brianne, the prognosis is increasingly hopeful.
Both antidepressant medication and cognitive-behavior therapy (talk
therapy that helps patients identify and deal with sources of stress) have
enabled many teenagers to focus on school and resume their lives. And more
effective treatment may be available in the next few years. The NIMH
recently launched a major 12-city initiative called the Treatment for
Adolescents With Depression Study to help determine which regimens—Prozac,
talk therapy or some combination—work best on 12- to 18-year-olds. Brent
is conducting another NIMH study looking at newer medications, including
Effexor and Paxil, that may help kids whose depression is resistant to
Prozac. He is trying to
identify genetic markers that indicate which patients
are likely to respond to particular drugs. |
Jonathan Haynes was diagnosed
with depression while in jail for dealing drugs. Now 18, he works as a
cook and lives with his family on San Antonio’s East Side |
|
Doctors hope that the new
research will ultimately result in specific guidelines for adolescents,
since there’s not much evidence about the effects of the long-term use of
these medications on developing brains. Most antidepressants are not
approved by the FDA for children under 18, although doctors routinely
prescribe these medications to their young patients. (This practice,
called “off-label” use, is not uncommon for many illnesses.) Many of the
drugs being tested—like Prozac and Paxil—are known as SSRIs, or selective
serotonin reuptake inhibitors. They regulate how the brain uses the
neurotransmitter serotonin, which has been connected to mood
disorders.
|
|
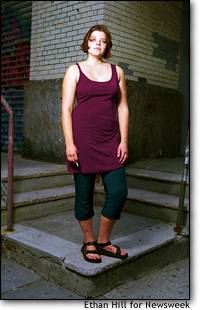
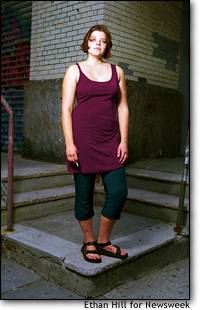
Gabrielle Cryan, now 19, got
her first Prozac prescription when she was a high school
senior
|
TRIAL-AND-ERROR THERAPY
Many depressed adolescents have a long history of trouble, which
often includes misdiagnosis and a lot of trial-and-error therapy that can
aggravate the social and emotional problems caused by the depression.
Morgan Willenbring, 17, of St. Paul, Minn., has suffered from depression
since he was 8, but school officials first thought he had
attention-deficit disorder. “I think that’s because they see that a lot,”
says his mother, Kate Meyers. “They tend to lump together what they see as
acting-out behavior.” It took more than two years to figure out a good
treatment regimen. Desipramine, one of the older antidepressants, didn’t
work. Then Willenbring spent six years on Wellbutrin, which was effective
but problematical because he needed to take it three times a day. “It’s
very easy to forget, which was not helping,” he says. When he missed too
many doses, he had trouble concentrating and got into fights at home. But
a month ago he switched to a once-a-day drug called Celexa and says he’s
doing better. He even managed to get through breaking up with his longtime
girlfriend without missing a day of school. |
|
The results of the NIMH
study may help make life easier for youngsters like Willenbring. The lead
researcher, Dr. John March, a professor of child psychiatry at Duke
University, says there is already evidence from other studies supporting
short-term behavioral therapy and drugs like Prozac and Paxil. But that
regimen works only in about 60 percent of cases, and almost half of those
patients relapse within a year of stopping treatment. “We’re hoping [the
study] will tell us which treatment is best for each set of symptoms,”
March says, “and whether the severity of symptoms biases you toward one
treatment or another.”
Until the results of
that study and others are in, parents and teenagers have to weigh the risk
of medication against the very real dangers of ignoring the illness. A
recent report from the Centers for Disease Control found that 19 percent
of high-school students had suicidal thoughts and more than 2 million of
them actually began planning to take their own lives. One of them was
Gabrielle Cryan. In 1999, during her junior year at a New York City high
school, “I obsessed about death,” she says. “I talked about it with
everyone.” With her parents’ help, she found a therapist just before the
start of her senior year who “put a name to what I’d been feeling,” says
Cryan. “My therapist made me realize it, face it and get over it.” She
also received a prescription for Prozac. Although she had some hesitations
about Prozac, “it really did help me,” she says. So did the talk therapy.
“The first part of the healing process—and I know this sounds corny—was
becoming more self-aware,” she says. The therapy helped her see that
“everything was not a black-and-white situation.” Before therapy, little
things would throw her into a funk. “I couldn’t find my shoe and the whole
week was ruined,” she says now with a laugh. “They taught me to get some
perspective.” And while her depression now is “nonexistent,” she knows
that she may have to face it again in the future. “We’re all a work in
progress,” Cryan says. “But I’ve picked up a lot of tools. When I feel
symptoms coming on, I can reach out and help myself now.” Stories like
hers are the successes that lead others out of the darkness.
With Brian Braiker in Boston, Karen Springen in
Chicago and Ellise Pierce in Dallas
© 2002 Newsweek, Inc.
|
|
|
|

 Eric Suarez,
17, who suffers from bipolar disorder, takes nine medications daily to
treat his depression-some for the symptoms and others to combat the side
effects of those drugs.
Eric Suarez,
17, who suffers from bipolar disorder, takes nine medications daily to
treat his depression-some for the symptoms and others to combat the side
effects of those drugs.  BRIANNE STARTED DRINKING and experimenting with drugs.
One Sunday she was caught shoplifting at a local store and her mother,
Linda, drove her home in what Brianne describes as a “piercing silence.”
With the clouds in her head so dark she believed she would never see light
again, Brianne went straight for the bathroom and swallowed every Tylenol
and Advil she could find—a total of 74 pills. She was only 14, and she
wanted to die.
BRIANNE STARTED DRINKING and experimenting with drugs.
One Sunday she was caught shoplifting at a local store and her mother,
Linda, drove her home in what Brianne describes as a “piercing silence.”
With the clouds in her head so dark she believed she would never see light
again, Brianne went straight for the bathroom and swallowed every Tylenol
and Advil she could find—a total of 74 pills. She was only 14, and she
wanted to die.