The National Tuberculosis Programme (NTP)
India's National Tuberculosis Programme (NTP) was
established in 1962 and provided a system 446 District TB Centres, 330 TB
clinics, and more than -47,000 hospital beds – for TB control throughout the
country. After more than three decades of operation, the NTP can justly claim
to have established an infrastructure for tuberculosis treatment in India.
However, with a treatment completion rate of only 30 percent, the programme did
not make a significant dent in the problem.
Part of the difficulty undoubtedly lies in the perceived
priority of tuberculosis in India. One study of the problem from the Indian
Institute of Management, Ahmedabad found that tuberculosis had a low priority
compared to other diseases; funding was disproportionately low; senior
programme leaders did not remain in place for long: health staff were pressured
by non-TB activities; patients experienced indifferent programme delivery; and
the visibility of TB in the media was low.
Until
recently, tuberculosis has had a smaller central budget than malaria, leprosy,
blindness, or AIDS. Only guinea worm, among the priority communicable diseases,
received less. Negative expectations about the TB programme have tended to
become self-fulfilling.
In 1992, a review of the National
Tuberculosis Programme by national and international experts - in coordination
with the World Health Organization and the Swedish International Development
Association - determined that the programme had not had the desired impact on
tuberculosis in India. The review noted inadequate budgets, a lack of coverage
in some parts of the country, shortages of essential drugs, poor
administration, varying standards of care at the district centres, unmotivated
and unevenly trained staff, lack of equipment, poor quality of sputum
microscopy, and focus on case detection without an accompanying emphasis on
treatment outcomes. There was a general consensus that, in a revised
tuberculosis control programme, the patient would have to be both the starting
point and the focus, It is therefore essential to understand the patterns of
diagnosis and treatment from the patient's perspective.
"Health-Seeking
Behaviour of Chest Symptomatics"
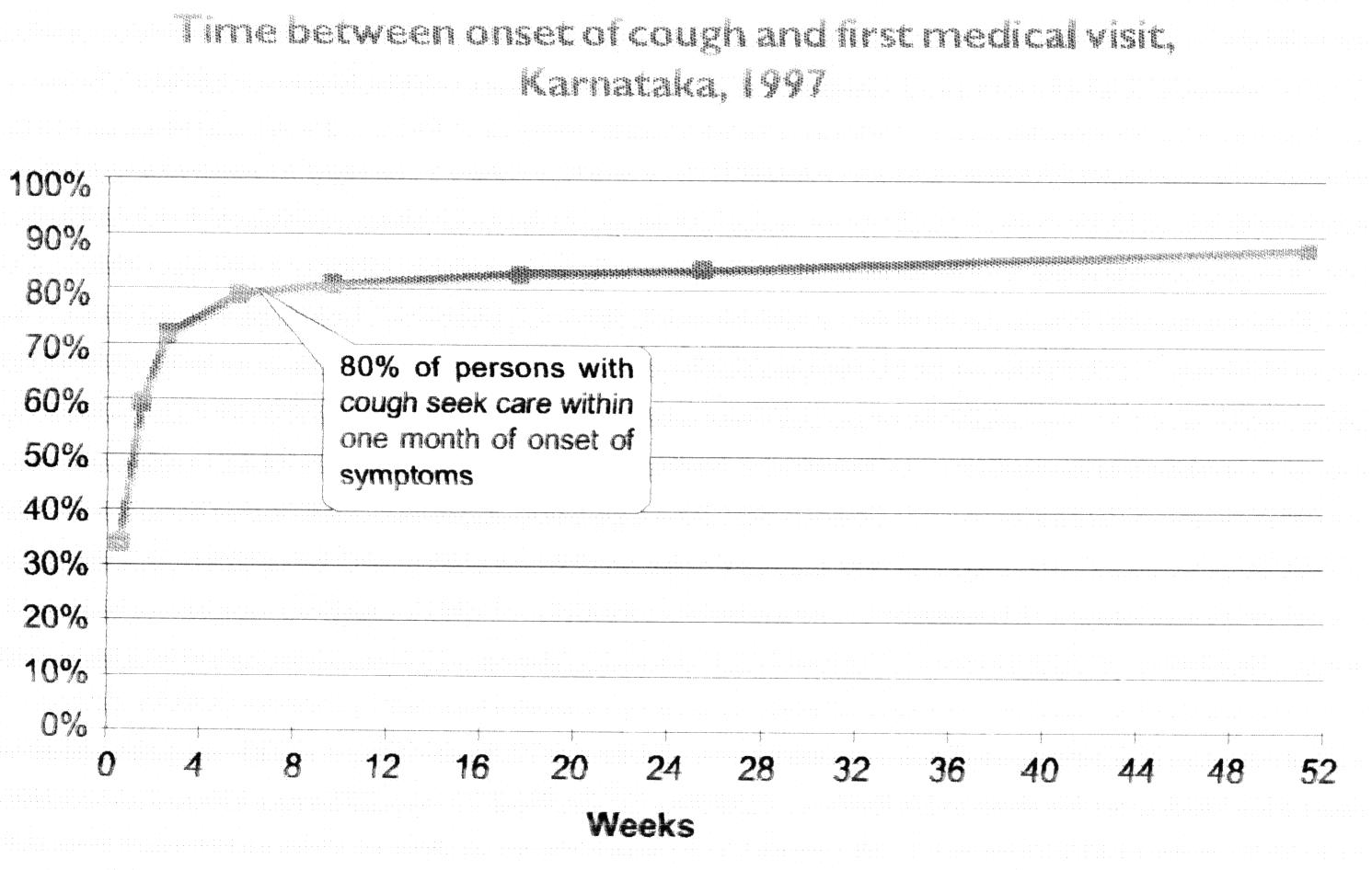
In India, the vast majority of
patients with active tuberculosis seek treatment for their disease, and do so
promptly. However, many patients spend a great deal of time and money
"shopping for health" before they begin treatment, and, all too
often, they do not receive either accurate diagnosis or effective treatment,
despite spending considerable resources. In a community-based systematic survey
in Karnataka, cough for three weeks or more was present in 1.4% of
people; rates increased with age, and were higher among males than among
females (See figure). Patients usually visit a number of health providers -
from general practitioners and general hospitals to practitioners of indigenous
medicines and even quacks. Unqualified rural practitioners are the first
point of contact for many TB patients.

This study also found that patients almost always seek care
promptly. The average time it takes for a patient to visit a health facility
after the appearance of symptoms was less than 2 weeks. Virtually all
symptomatic patients who sought care did so within one month of the onset of
symptoms. In areas with better performing health systems, patients sought care
even more promptly. The only sub-group which did not seek care promptly was
elderly, non-literate males.
Delay between the onset of symptoms and the start of
effective treatment is important in the control of tuberculosis because during
this rime patients are most infectious. Most delay in diagnosis is on the part
of the health system, not patients.
One barrier to treatment is the stigma that is still
associated with tuberculosis. In many parts of India, this remains a serious
problem.
In one recent study, researchers interviewed several
hundred patients and their families and found that most patients felt
uncomfortable talking about tuberculosis. Several patients denied that they
were suffering from the disease or taking treatment for it, and some even
refused to mention tuberculosis by name. Patients frequently attempted to hide
their disease from their family and community by registering under false names
at tuberculosis clinics or by denying their identity when confronted by
interviewers.
Similarly a study by the Indian institute of Management
found that most patients were reluctant to admit that they had TB because they
feared stigma, and they preferred not to discuss the disease in the presence of
family or neighbors. This was more so in urban than in rural areas. Family support
for treatment was more frequent among cured patients than among those who had
defaulted.
|
First action taken by chest symptomatics
|
|
|
Mysore district
|
Raichur district
|
Tamil Nadu
|
Delhi
%
|
Average
%
|
|
Rural
%
|
Urban
%
|
Rural
%
|
Urban
%
|
Rural
%
|
Urban
%
|
|
Private provider
|
48
|
76
|
93
|
74
|
48
|
57
|
55
|
64
|
|
Government facility
|
51
|
22
|
5
|
25
|
46
|
32
|
21
|
29
|
|
Self-medication
|
--
|
--
|
--
|
--
|
4
|
8
|
10
|
3
|
|
Home remedies
|
--
|
--
|
--
|
--
|
1
|
2
|
6
|
1
|
|
Others
|
1
|
2
|
2
|
1
|
1
|
1
|
8
|
2
|
|
Total taking
action
|
83
|
85
|
90
|
85
|
63
|
80
|
82
|
81
|
|
No action prior to
interview
|
17
|
15
|
10
|
15
|
37
|
20
|
18
|
19
|
|
|
|
|
|
|
|
|
|
|
The majority of TB patients in India who seek help first
consult one of India's 10 million private medical practitioners (See previous
tables). In studies that assessed the health-seeking behaviour of chest symptomatics in rural Karnataka and Tamil Nadu,
and in urban Karnataka, Tamil Nadu and Delhi, researchers found that 64 percent
first sought help from a private provider Only 29 percent went to a government
facility on the first visit. Ramana et al. found that 80 percent of all private
practitioners in their study areas in rural and urban Andhra Pradesh were
treating tuberculosis.
The major causes patients gave for seeking private
providers were proximity and convenient working hours; while the main reason
for going to government facilities was free treatment.
Studies have shown that, despite having limited
resources, most patients are not promptly diagnosed and treated, and therefore
go from one doctor to the next before a diagnosis is firmly established and
treatment begins.
In one study, the average number of health providers
visited by patients from the time they developed symptoms to the time they
registered at a TB clinic was 2.5 for urban patients and 4.0 for rural patients.
Not only did this increase the cost of treatment, increasing debt, but it also
delayed prompt initiation of treatment, thus avowing disease to spread further
in the community.
The total cost incurred by patients shopping for care was
about Rs 1000 ($30) in urban and Rs 630 ($18) in rural Karnataka, and about Rs 550 ($16) and Rs 400 ($11)
in urban and rural Tamil Nadu.
All too often, health providers
fail to diagnose the disease correctly, thereby delaying the start of treatment
and perpetuating the chain of infection in the community
|
Provider consulted first by patients with
tuberculosis
|
|
Provider Consulted First
|
Medak (rursal)%
|
Hyderabad (urban)%
|
Unqualified neighborhood doctor
|
7.1
|
1.5
|
|
Qualified neighborhood doctor
|
25.7
|
55.2
|
|
Doctor (not aware of qualifications)
|
41.5
|
20.9
|
|
Specialist in TB/Chest Diseases
|
0
|
.7
|
|
Specialty Hospital
|
8.6
|
0
|
|
Clinic/Dispensary/PHC
|
4.3
|
3
|
|
Hospital
|
1.4
|
14.9
|
|
TB Clinic/Hospital
|
11.4
|
3.8
|
Source: Mapping of TB Treatment Providers at Selected Sites in Andhra
Praradesh State,
Many providers do not confirm their diagnosis of pulmonary
tuberculosis by sputum examination, relying instead on chest radiographs and
thus often incorrectly diagnosing patients to have tuberculosis, in one study
in Bombay, only 39 percent of doctors used sputum examination to confirm the
diagnosis of tuberculosis. Studies in Delhi, Karnataka, and Tamil Nadu revealed
that, even after multiple visits, less than one third of patients underwent
sputum smear examination. In one study, even after 8 encounters with the health
system, less than one third of patients had undergone even a single sputum
examination, despite spending 1-6 months of their income, in rural areas, lack
of access to effective diagnosis and treatment was even more pronounced (See
figure).
Even when tuberculosis is diagnosed by private
practitioners, prescribing practices vary widely. A study of 100 private
doctors in Bombay, found that there were 80 different regimens, most of which
were either inappropriate or expensive, or both. In a similar survey in Pune,
113 doctors prescribed 90 different regimens. Private doctors seldom felt that
it was their duty to educate the patients about TB and never made attempts to
contact or trace patients who had interrupted treatment. Virtually no
individual patient records are maintained by private physicians.
Even when patients are eventually diagnosed and then
prescribed the correct treatment regimen, many discontinue it if they are not
supported and monitored throughout the treatment period. The two main reasons
offered by the majority of those who stopped treatment were that they felt
better and had therefore discontinued their drugs, and that there was too much
cost and trouble associated with getting an uninterrupted supply of drugs.
Estimates in India indicate that, of every 100 infectious
tuberculosis cases in the community, about 30 are identified in the public
sector, of which at most 10 are cured; similarly, about 30 are identified in
the private sector, of which at most 10 are cured. Hence, not more than 20
percent of patients who develop tuberculosis in India each year are cured. Many
of the remaining patients remain chronically ill or die slowly from the
disease, infecting others with strains of the disease which may have developed
drug resistance.
Despite these serious shortcomings, there are signs of
hope. Most practicing physicians reported that they would be interested in
receiving training on DOTS, and most were willing to have their offices used as
centres for treatment observation for their patients, free of charge.
How is TB disease treated in India?
There are many possible anti-TB treatment regimens. The World Health
Organization (WHO) and the International Union against Tuberculosis and Lung
Disease (IUATLD) recommend standardized TB treatment regimens.
The most common drugs used to fight TB (when used in combination of more
than one drug, called a "regimen") are:
· isoniazid
(INH or H)
·
rifampicin (R)
·
pyrazinamide (Z)
·
ethambutol (E)
·
streptomycin (S)
Based on case- definition, a TB patient may fall into any one of the
following four categories for treatment. The categories are numbered in order
of priority. The highest priority for treatment is Category 1 patients and the
lowest priority is Category 4:
Category 1: New cases who
are smear-positive, or seriously ill patients who are smear-negative or who
have extra-pulmonary disease.
Category 2: Re-treatment
cases including patients with relapse, treatment failure and those who return
to treatment after default. Such patients are generally sputum-positive.
Category 3: Patients who
are sputum-negative, or who have extra-pulmonary TB and are not seriously ill.
Category 4: Chronic cases,
still sputum-positive after supervised re-treatment
Treatment regimens usually comprise two phases: the Intensive phase and the
continuation phase. There are several possible regimens for treating each
category of TB. Suggested alternatives are given in the following table.
However, it is important to stress that in a given country, the
regimen recommended by the National TB Programme, which is described in the NTP
Manual, should be followed.
Table 1 Possible alternate
treatment regimens for each treatment category
|
TB treatment category
|
Alternative TB treatment Regimens
|
|
Initial Phase
(daily or 3 times a week)
|
Continuatioin phase
|
|
I
|
2 EHRZ (SHRZ)*
2 EHRZ (SHRZ)
2 EHRZ (SHRZ)
|
6 HE*
4 HR
4 H2R3
|
|
II
|
2 EHRZ (SHRZ)/ 1
HRZE
2 EHRZ (SHRZ)/ 1 HRZE
|
5 H3R3E3
5 HRE
|
|
III
|
2 HRZ
2 HRZ
2 HRZ
|
6 HE
4 HR
4 H3R3
|
|
IV
|
Not Applicable
(Refer to WHO guidelines for use of
second-line drugs in specialized centres )
|
* A standard code is used for
each drug. For example, the regimen of 2HRZE(S)/4HR has two phases
· The
intensive phase (2HRZE) means daily treatment with a combination of four drugs
for two months: isoniazid (H), rifampicin (R), pyrazinamide (Z) and ethambutol
(E). The last drug (E) and streptornycin (S) can be interchanged where either
one or the other of the two drugs is available.
·
The continuation phase (4HR) means daily treatment with
isoniazid (H) and rifampicin (R) for four months
For the regimen 2HRZE(S)/4H3,R3, the abbreviation H3R3 means a treatment
three times a week with both isoniazid and rifampicin.
|
Anti-TB Drug
(Abbreviation)
|
Recommended Dose (mg/ kg)
|
|
|
Daily
|
Intermittent
3x /wk
|
|
Isoniazid(H)
|
5(4-6)
|
10(8-12)
|
|
Rifampicin (R)
|
10(8-12)
|
10(8-12)
|
|
Pyrazinamide (Z)
|
25(20-30)
|
35(30-40)
|
|
Streptornycin (S)
|
15(12-18)
|
15(12-18)
|
|
Ethambutol (E)
|
15(15-20)
|
30(25-35)
|
|
Thiacetazone(T)
|
2.5
|
Not Applicable
|
All these anti-TB drugs should be given as as a single daily dose. Direct
observation is recommended for all patients and is particularly essential when
intermittent regimens are used. Thiacetazone is not effective when given
intermittently and is not recommended for use in high HIV prevalence areas.
The
side-effects of anti-TB drugs
The side effects of individual anti-TB drugs are shown in the table below.
They are classified as minor or major. In general, a patient who develops minor
side effects should continue the anti-TB treatment, usually at the same dose or
if necessary at a reduced dose. The patient should also receive symptomatic
treatment. If a patient develops a major side effect, the treatment or the
offending drug should be stopped.
|
Table 2 Side-effect of anti-TB drugs
|
Side-effects
|
Drug(s) probably responsible
|
Minor
|
|
1
|
anorexia, nausea, abdominal pain
|
|
2
|
joint pain
|
|
3
|
burning sensation in the feet
|
|
4
|
orange/ red urine
|
|
rifampicin
pyrazinamide
isoniazid
rifampicin
|
Major
|
|
1
|
itching of skin, skin rash
|
|
2
|
deafness
|
|
3
|
dizziness
|
|
4
|
jaundice
|
|
5
|
vomiting and confusion
|
|
6
|
visual impairment
|
|
7
|
shock, purpura, acute renal failure
|
|
thiacetazone (streptomycin)
streptomycin
streptomycin
most anti-TB drugs (esp. H,Z,R)
most anti-TB drugs
ethambutol
rifampicin
|
Are the side-effects or toxicity
due to anti-TB drugs more common in HIV-positive Individuals?
Adverse reactions are
generally more common in HIV-positive than in HIV-negative TB patients. Most
reactions occur in the first two months of treatment. Skin rash and hepatitis
are more common and most often attributed to rifampicin. The usual drug
responsible for fatal skin reaction such as exfoliative dermatitis,
Steven-Johnson syndrome, and toxic epidermal necrolysis is thiacetazone.
Therefore, thiacetazone should never be given to HIV-positive TB patients. From
a programmatic point of view, thiacetazone should not be prescribed in areas
where HIV prevalence is shown to be high.
Key Findings and implications for
Action
Patients with symptoms of TB seek care promptly - but in
both the public and the private system, they are neither reliably diagnosed nor
effectively treated. Where services are better people use them more promptly
and more often despite 8 encounters with the health system and the expenditure
of 1-6 months' wages, less than one third of patients with symptoms of TB had
undergone even a single sputum examination for AFB! in both public and private
sectors, successful treatment of tuberculosis is the exception rather than the
norm.
• The behavior of patients does
not need to be changed - the health system's response to this behavior must
improve.
• Diagnostic
practices need to be strengthened urgently. In both public and private primary
health care systems health workers need to "Think TB" and ensure that
all adult patients are asked whether or not they have cough for 3 weeks, and,
if they do, that they undergo 3 sputum examinations in a good quality
laboratory.
• Programme managers need to publicize the location and
availability of free sputum microscopy centres, and the fact that 3 sputum
samples should be examined if patients have cough for 3 weeks or more.
• Programme managers need to involve both qualified and
unqualified practitioners to refer patients for diagnosis.
• Practicing
physicians should ensure that every patient with symptoms of TB undergoes 3
sputum examinations in a quality-controlled laboratory, preferably by referring
such patients to an RNTCP microscopy centre.
• In
public and private sectors, improved interpersonal communication, standardized
treatment, direct observation at a time and place convenient to patients, and
systematic monitoring and accountability are needed urgently.