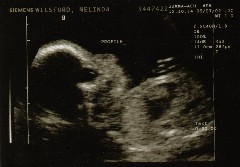
Abigail's Story - Diagnosis and Preparation
When we found out in January that we were expecting our 3rd child in September 2002, we were really excited. We started thinking about moving our daughter, Sarah, then 18 months, out of the crib so the new baby could use it. And Nathan (4) would get to move into a new bedroom as well. I was told that since I had 2 previous c-sections that this one would also be a c-section. That would work out well since we would schedule it ahead of time and be able to arrange childcare. Despite the fact that I was 39, we did not opt for AFP testing or amniocentesis, since we knew that due to our faith in God we would not terminate this pregnancy even if problems were found.

Our Introduction to Trisomy 18
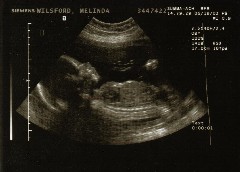
Before the ultrasound, the genetic counselor explained that this type of cyst is not a problem itself; in fact, it would go away before birth. Many healthy babies have these; however, it has been observed that a high percentage of babies with a particular chromosome disorder show this type of cyst. And this was our introduction to the world of Trisomy 18 (or Edwards Syndrome), which occurs when a baby has 3 chromosomes in the 18th position instead of the usual two. This condition affects many parts of the body and is associated with a very high incidence of pregnancy loss and neonatal death. However, the presence of the choroids plexus cysts alone indicates less than a 1% chance of chromosome problems, no more than the risk already associated with mothers my age (39). But she explained that if additional abnormalities (or markers) for a chromosome problem were found, the chance of a chromosome abnormality would be significantly higher. This was all somewhat overwhelming, but logic told us that the odds still were overwhelming in favor of a healthy child.
The fetal echo took over an hour, and I began to think the doctor had found something wrong. Then he took us into a conference room to explain what he found. He drew diagrams of a normal heart and of our baby’s heart. His main concerns were a VSD (a small hole between the pumping chambers) and a possible coarctation after birth. The VSD would probably require surgery after 3-6 months, and coarctation would require surgery within a day or two after birth. These problems would be correctable, but we were not happy to find that she had a heart problem. The doctor strongly encouraged us to have an amnio to rule out chromosome problems, since that would change the course of treatments. So we went and had the amnio.
At this point, we did a lot more research on Trisomy 18 and I did a lot of crying and imagining. But I was still figuring it wasn’t likely to be the diagnosis, based on the odds. In fact, when I called my mother to tell her about what was found, I didn’t mention what the chromosome problem was or it’s severity, figuring there was no point in worrying her unless we got a positive diagnosis of Trisomy 18.
It was hard waiting for the results, even though I really felt everything would be fine. When they came in, the doctor didn’t beat around the bush. He said the baby had an extra chromosome in the 18th position. He also asked if the genetic counselor had explained this to us. I replied that she had and said, “it’s pretty bad isn’t it”. What an understatement! He said he would have them call me. I was stunned and devastated! Against the odds, she did have Trisomy 18. I called my husband and told him. I don’t really remember much about the call with the counselor. She offered to send some resource materials, asked if we had any questions, and reiterated some of what we had discussed earlier. I was pretty strong about it overall, but I did start crying a couple of times. After the call, I called a coworker with whom I had been talking all along. She came down and let me talk a little and cry a lot. Then I asked her to tell my coworkers and I went home.
Dealing with the diagnosis
It was Independence Day weekend, so the family was all together for the long weekend. I spent hours on the internet looking at Trisomy 18, and everything pointed to the fact that our baby was most likely to be stillborn, or if she were born alive, she would likely live only days, hours, or even minutes. How do I even deal with this? I spent a lot of time hugging my other children, praying, and of course, crying. The praying was hard, because I didn’t know what to pray for – what would be the best for her, our other kids, and us? I really longed for her to be born alive so we could at least have some time with her, but I had to be ready if she wasn’t. So, once again, we went with the odds and tried to prepare ourselves for her to be stillborn or for us to have only minutes with her. And we prayed for the strength to deal with whatever outcome we got.
The emotions were really intense, and they kept changing. About 3 days after the diagnosis, we decided to name her Abigail Grace. We also talked about whether to cremate or bury her, what type of memorial to do (build a playground for other kids to enjoy), and other issues relating to the impending death of our baby. And I was amazed at how angry I was about being pregnant and how much I hated it at that moment. I felt like it was a constant reminder to me and everyone else who knew that my baby was going to die. I also felt like it was such a waste to have to go through all of it when my baby was going to die.
And it was almost unbearable to think about those who didn’t know and were going to ask me cheerful questions about the pregnancy. How could I endure this until she was born? I just wanted it to be over. I probably cried harder and longer then than any other time during this whole journey. Eventually, I got exhausted from crying and actually felt a lot better. Later that evening, searching the internet as usual, I found the Carrying to Term Pages and saw a section about early emotions that said that it is common to hate the pregnancy for awhile, but that it would pass quickly. That made me feel better (hopeful) about it, and that feeling did pass in a couple of days.
How we explained Trisomy 18 to our friends.
We then set out to learn as much as possible about the situation so we could make the best possible choices regarding Abigail’s care. We met with a geneticist who explained all the possible effects of Trisomy 18 on each of the body’s systems, starting at the top and moving down. He explained that a T18 baby’s brain is not properly developed; the neurons don’t make it all the way to the outside of the brain but remain in little clusters. One key thing was when he explained that a Trisomy 18 baby has a susceptibility that a healthy baby doesn’t. That is, a T18 baby will succumb to things that would not be fatal to a healthy baby. This was important for us to hear, because it helped us understand that fixing some of our baby’s problems would not be helpful to her because the Trisomy 18 itself would not be fixable.
During that meeting, we expressed our desire to provide comfort care for the baby, and we decided to create a birth plan to ensure that we could keep her as comfortable as possible. While researching the birth plan, I found a message board on the internet for Trisomy 18 that was a real Godsend. (That message board was part of what has now become the Trisomy 18 Foundation, where I received invaluable support throughout my entire journey - and where I continue to give and receive support today). Reading the stories there, it also cemented the reality of Trisomy 18: many of the babies were stillborn, and of those born alive, most only lived minutes or hours. This again reinforced for me the need to have a birth plan that makes the most of the first minutes after the birth.
Telling the other kids
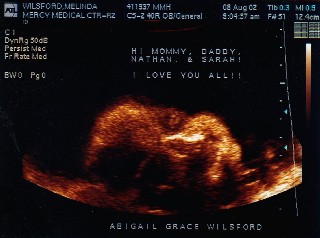
At the same time, we decided to help Nathan and Sarah get to know her and be ready for what would happen. We encouraged them to lean over mommy’s tummy and say, “Hello, Abigail!” and “Wake Up, Abigail!” At first, it was a very forced, false cheerfulness that we had with the kids. It was so painful to talk to her ourselves and to have them do it. But over time, it became natural and we started thinking of her as baby Abigail who we loved, not as baby Abigail who has Trisomy 18. The kids started hugging her and telling her “goodbye” when I left for work, and soon it just made me joyful and happy to see their love and to think of her, not painful like before. We told Nathan that Abigail was sick and might not live, and so at first whenever we talked about Abigail, he would ask, “but what about ‘might not live’?” One day, he asked, “if she dies, will we have another baby in a few months?” He also asked how long will she live? And one time he said, “maybe she’ll be well for one day.” Sometimes it made me cry to answer his innocent questions and to think that he had to be asking those questions at his age. But he handled it very well, knowing that Abigail would be going to heaven to be with Jesus and that someday “he’d be old enough to go be with Jesus, too”.
We began to appreciate the last few weeks of “normalcy” that we would have; we were a family enjoying the baby that mommy was going to have, and our lives were still pretty much the same as before – for awhile. But it was still really hard, mainly because there was so much uncertainty, so much we didn’t know. Will she live at all? Will we have minutes or hours? Days or weeks? Will we bring her home? Thinking about the possibilities and trying to prepare ourselves was overwhelming and exhausting. We stopped even trying to decide what to wish for; we just kept praying that God would give us the wisdom to make the right decisions for her care and for helping our other kids deal with it, and that he would give us the strength to deal with whatever happened.
A lot of resources were pulled together to create the birth plan: internet, Fetal Treatment Center, palliative care specialists. And we were blazing new territory at our hospital; usually this type of situation is transferred to a larger hospital that sees this more frequently. Some of the things we wanted were out of the ordinary and required us to make arrangements ahead of time. So we had to meet with the neonatologists and the pediatrician that would be handling Abigail’s palliative care. To complicate things, I injured my back in early August and was literally confined to bed for over 2 weeks with terrible sciatica. So we did some meetings by phone and had to take me in a wheelchair to others, since I couldn’t stand or walk more than a couple of feet at a time. But finally, we had arrangements finalized: September 4th was the date for my scheduled c-section (over 2 weeks ahead of my due date). On August 26th, we met with the pediatrician to discuss Hospice and home care should we bring Abigail home, something we had not really thought about yet. We were finally ready to try to relax until the 4th.
In addition to the actual birth plan, we had decided we would do comfort care for Abigail. Our decision was in large part based on a strong faith in God and a knowledge that Abigail would only be healthy and whole once she was in heaven. We felt that putting her through painful procedures or tests just to keep her with us here on earth for a few more days or weeks was selfish; that is, it would be only for our benefit, not hers. So we decided we were not going to put her through any surgeries, but would try to make her feel as comfortable and loved as possible while she was with us. As hard as it would be to let her go, we will get to see her again for eternity in heaven!
Continued with Abigail's birth....
