EMS Update:
Anatomy & Physiology of the Heart
Dispatch
THE STRUCTURE OF THE HEART
- The size and position of the heart
Despite its heavy workload, the heart is not a large organ. It is about the size of the person’s clenched fist and weighs 10 to 12 ounces. It is hollow and roughly conical in shape, with the narrow end pointed downward, to the left, and slightly forward. Its location in the chest cavity is just to the left of the midline, behind the sternum and between the second and sixth left ribs (see Figure 1).
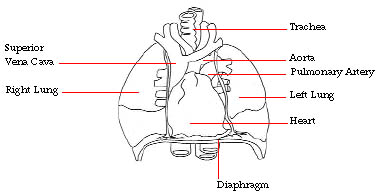
Figure 1: Position of the heart in the chest viewed from the front.
The wall of the heart consists of three layers: the pericardium, a fibrous sac surrounding the heart whose inner lining is a thin, transparent membrane covering the outside of the heart muscle; the endocardium, the delicate innermost lining of the heart; and, the myocardium, the thick muscular layer that separates the two linings. The myocardium is a specialized type of muscle that is unique to the heart and responsible for its contraction.
The heart has four cavities or chambers. Two of these are thin-walled receiving chambers, the left and right atria (singular, atrium), and two thick-walled pumping chambers, the ventricles. Actually, the heart consists of two parallel pumps that work simultaneously. The right-sided pump receives deoxygenated blood from the veins and pumps it to the lungs where it is re-supplied with oxygen. The left-sided pump receives the reoxygenated blood from the lungs and pumps it through the arteries to the rest of the body (see Figure 2).
The heart contains four valves. There is a valve between the right atrium and right ventricle, the tricuspid valve, and one between the left atrium and the left ventricle, the mitral valve. These valves are open when the ventricles are filling and receiving blood from the atria, but close when the ventricles contract and are so structured that they prevent back-flow or regurgitation of blood from the ventricle into the atrium. The right ventricle pumps blood into the pulmonary artery on its way to the lungs. There is a valve, the pulmonic valve, at the outflow area of the right ventricle. It opens when the ventricle contracts, but closes during diastole, thus preventing regurgitation of blood from the pulmonary artery back into the right ventricle. A similar valve, the aortic valve, is present at the outflow area of the left ventricle. It is open when the left ventricle contracts sending blood into the aorta, but closes during diastole so that blood cannot regurgitate from the aorta back into the left ventricle. The contraction of the ventricles and the closure of the valves contribute to the sounds of the heart, often described as lubb, the contraction or first sound, and dupp, the second cardiac sound (see Figure 2).

Figure 2: View of the opened heart from the valve showing valves and main blood vessels entering and leaving heart.
The flow of blood through the heart
Blood enters the right atrium from the veins and passes through the tricuspid valve into the right ventricle. The right ventricle contracts, expelling blood through the pulmonic valve into the pulmonary artery on its way to the lungs. As the right ventricle contracts, the tricuspid valve closes, preventing regurgitation of blood into the right atrium. Following right ventricular contraction, the pulmonic valve closes to prevent regurgitation of blood back into the right ventricle. Reoxygenated blood returns from the lungs by way of the pulmonic veins and enters the left atrium. Blood flows through the open mitral valve into the left ventricle. After the left ventricle fills, it contracts sending blood through the aortic valve into the aorta and the rest of the body. As the left ventricle contracts, the mitral valve closes to prevent regurgitation into the left atrium. After left ventricular contraction, the aortic valve closes to prevent regurgitation of blood from the aorta back into the left ventricle.
After returning from the pulmonary circulation, the oxygenated blood begins its systemic circulation. Systemic (peripheral) circulation is that part of circulation in which blood is transported to all body tissues and returned to the heart. It begins when oxygenated blood leaves the left ventricle. When the ventricles relax, oxygenated blood flows from the left atrium through the mitral valve into the left ventricle. When the ventricles subsequently contract, this blood is pumped with considerable force through the aortic valve into the major artery of the body, the aorta.
As the aorta descends, it branches into several smaller arteries. Some of these arteries, such as the carotid arteries, carry blood to the head and neck. Other arteries, such as the subclavian arteries and the femoral arteries, carry blood to the upper and lower extremities, respectively.
From these arteries, blood enters the arterioles and then the capillaries, where oxygen is exchanged for carbon dioxide and nutrients for metabolic wastes. The deoxygenated blood that has been used by the body then travels back to the heart by way of the venules and veins. It finally empties into two principal veins: the superior vena cava, which carries blood from the upper portion of the body; and the inferior vena cava, which carries blood from the lower portion of the body. Blood from both the superior and inferior vena cavae enters the right atrium, where systemic circulation ends. With the next heart relaxation, the blood again flows from the right atrium through the tricuspid valve into the right ventricle, and the cycle of pulmonary circulation to systemic circulation is repeated.
The following diagram summarizes the flow of blood through the body, tracing it from the peripheral venous system into the heart, through the pulmonary circulation, back to the heart, to the systemic circulation, and back again to the heart (see Figure 3).
Venous blood enters right atrium from venae
cavae
![]()
Blood enters right ventricle through tricuspid valve
![]()
Right ventricle contracts, sending blood through the pulmonic valve into pulmonary artery
![]()
Blood enters pulmonary capillary system, where gas exchange takes place
![]()
CO2 in pulmonary venous capillaries exchanges for O2 in pulmonary alveoli (air spaces)
![]()
Oxygenated blood returns to left atrium via pulmonic veins
![]()
Blood enters left ventricle through mitral valve
![]()
Left ventricle contracts, sending blood through the aortic valve into systemic circulation
![]()
Gas exchange occurs within capillary system of peripheral circulation; O2 is released into
tissues and CO2 enters the deoxygenated venous circulation for return to the heart.
Figure 3: Tracing the flow of blood through the heart and the pulmonary and systemic circulation.
The circulation of the heart (coronary circulation)
The heart also has its own important blood supply, the coronary circulation. The two main coronary arteries, the left and the right coronary arteries, branch from the aorta as it leaves the heart. The left coronary artery then divides into the circumflex artery and the left descending artery. These three arteries are the principal coronary arteries and they, in turn, give rise to numerous branches guaranteeing the heart a rich supply of blood and oxygen (see Figure 4).
The major coronary arteries lie on the surface of the heart. From them, smaller arteries pass into the myocardium, ultimately forming arterioles and capillaries and comprising the collateral circulation. When needed, coronary arterioles have the ability to increase the size and number of collateral vessels. This forms a valuable increase in the blood supply in the event of an occlusion of a coronary artery.
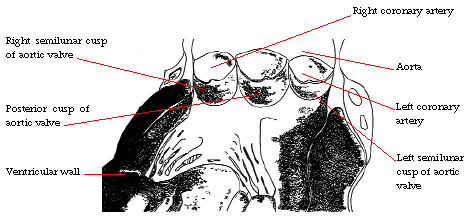
Figure 4: The Coronary Circulation.
A decrease in the oxygen supply to the heart as a result of narrowing or complete obstruction of a coronary artery results in angina pectoris if the obstruction is incomplete and transient. When a portion of the myocardium is deprived of blood permanently, that portion of the myocardium sustains myocardial infarction due to death of that portion of the myocardial muscle.
The nervous system of the heart
Although the heart has the remarkable property of automaticity and is capable of contracting on its own, it is supplied with two sets of nerves to augment its work. There are sympathetic nerves that stimulate the heart causing it to beat faster and with greater strength, and parasympathetic nerves that calm the heart and slow its rate. These nervous systems carry impulses from the brain and elsewhere in the body that help the body respond and adjust to internal and external factors. Both systems respond to a variety of drugs that may be used in the treatment of various cardiac disorders and hypertension.

Anatomy & Physiology of the Heart
Overview of the Cardiovacular System
Hemodynamics of the Cardiac System