EMS Update:
Anatomy & Physiology of the Heart
Dispatch
The vascular system is divided into three components. The arterial system is responsible for the delivery of blood and oxygen to every cell, tissue and organ in the body. The arteries carry blood away from the heart. Veins comprise the venous system that is responsible for returning deoxygenated (deprived of oxygen) blood from the tissues and organs back to the heart. The capillary system links the two systems together and is responsible for the exchange of oxygen for carbon dioxide at the cellular level.
The vascular system is not a passive system of pipes, but actually plays a critical role in supplementing the action of the heart in the distribution of blood. Its status also plays a major role in the determination of the blood pressure.
aorta, the largest blood vessel in the body. The aortic valve is situated at the entrance to the aorta. During left ventricular systole, the valve opens, allowing the free flow of blood into the aorta. During diastole, the relaxation and refilling stage of the cardiac cycle, the aortic valve snaps shut, preventing regurgitation of blood from the aorta back into the left ventricle. Anatomically, the aortic valve consists of three cusps (posterior, right, and left) that come together during diastole to completely occlude the valve and prevent regurgitation. Because the edge of each cusp is in the shape of a half moon, the valve is sometimes called the semilunar valve (see Figure 6).
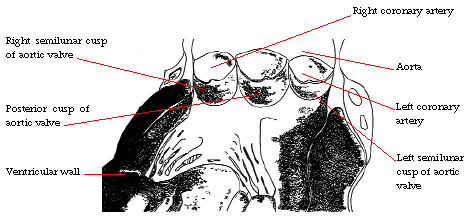
Figure 6: Base of the aorta showing anatomy of the aortic valve
Within the cavities formed by the right and left aortic cusps are the origins of the left and right coronary arteries. These are the arteries which branch to form the coronary circulation of the heart muscle and provide oxygenated blood to the heart muscle. Shortly after leaving the heart, the aorta arches to the left and sends large branches to the neck and head and to the upper extremities. The large arteries supplying the neck, head and brain with blood are called the carotid arteries. Their strong pulsations can be felt in the neck on both sides of the larynx. The aorta then descends down the back of the body in front of the spine, supplying branches to the chest and to the organs in the abdomen. In the pelvis, the aorta splits into two large branches, each supplying one of the legs with blood.
Figure 7 illustrates the major components of the arterial system.

Figure 7: The arterial system
As the arteries approach their goals, they get increasingly smaller and are called arterioles. Finally, they attain a thread-like diameter and are called capillaries.
If one examines the wall of an artery under the microscope, three layers are apparent. The intima is the innermost layer of the artery and is composed of endothelium, the delicate inner lining of the blood vessel. It is the endothelium that becomes involved with atherosclerosis, commonly referred to as hardening of the arteries. The middle layer of the arterial wall, the media has a layer of elastic tissue which is capable of decreasing and increasing the caliber of the blood vessel and thus controlling the flow of blood through it. The media of the large arteries also have a layer of . The arterial elastic and muscular tissues play important roles in supplementing the heart in the propulsion of blood through the vascular system. The nervous system and circulating hormones also play important roles in this action. The outer arterial wall layer, the adventitia, is composed of protective fibrous tissue.
Figure 8 depicts a microscopic view of the wall of an artery.
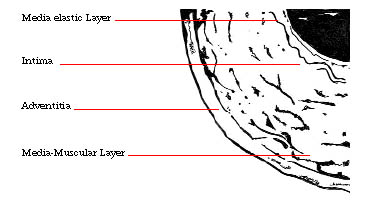
Figure 8: Microscopic view of the wall of an artery
Vasoconstriction is the term applied to constriction of a blood vessel. Vasoconstrictor substances are formed within the body, especially in the kidneys and adrenal glands. They play an important role in the control of blood pressure. Vasoconstriction causes an increase in blood pressure by increasing the resistance against which the heart has to work. The administration of vasoconstrictors is helpful in raising blood pressure and in the control of bleeding.
Vasodilatation is the term applied to dilatation of the blood vessels. This also occurs within the body under certain circumstances, causing a fall in blood pressure. Vasodilatation plays a role in the development of circulatory shock. Vasodilators are important therapeutic agents in the treatment of hypertension.
Both vasoconstriction and vasodilatation are under the control of ner-vous and hormonal influences over which we have little or no voluntary control.
The venous system is responsible for the return of blood from the tissues and organs of the body to the heart. The blood carried by the venous system has been depleted of oxygen in exchange for carbon dioxide (CO2). The transport of the blood from the heart to the lungs for replenishment of oxygen is considered by some as part of the venous system.
For the most part, arteries and veins travel and branch out through the body side-by-side, similar to the opposite sides of a highway with the traffic (or blood) flowing in opposite directions. In many instances, arteries and veins share the some name. All venous channels from the head and chest lead into the superior vena cava. Blood from below the chest drains into the inferior vena cava. Both of these large veins empty into the right atrium from which their contents are passed into the right ventricle. Right ventricular systole then pumps the blood to the lungs by way of the pulmonary arteries.
There are striking anatomical and physiological differences between arteries and veins. Whereas arteries are strong, muscular and elastic, veins are more delicate in structure and to a significant degree, lack the elasticity and muscular power of the arteries. They have a limited capability for vasoconstriction, but have a prominent capacity for vasodilatation. Arterial blood flow is much faster than venous blood flow because it reflects the power of the left ventricular contraction as well as the artery's own capability for contraction. Arterial bleeding is pulsatile, again reflecting the contraction of the left ventricle, whereas venous bleeding is slower and steady in character. In some of the major arteries, blood moves at a rate of over a foot a second, whereas the flow rate in veins is about 4 inches per second. Contraction of the muscles surrounding a vein assists in promoting venous blood flow. This mechanism is sometimes referred to as the venous pump. The venous pressure varies throughout the body, depending on the position of the individual and the site of measurement. It averages 50 to 100 mm of water, much lower than the pressure of 120 mm of mercury seen in arteries during systole. Arterial blood is much brighter and redder than venous blood because of its oxygen content.
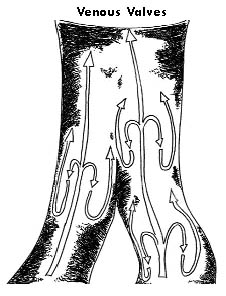
To prevent the reversal of the flow of venous blood, veins have valves that prevent this from happening. For example, standing in the upright position for a prolonged period would be expected to increase the pressure in the veins of the leg and promote backflow of blood (See Figure 9). The venous valves prevent this. Unfortunately, the valves are prone to damage and this may result in edema (swelling), and the presence of permanently dilated veins (varicose veins).
The veins have a greater capacity to widen or dilate than do arteries. Because of this, the volume of blood in our venous system is 2 to 2 1/2 times that in the arterial system. This pool of blood acts as an important reservoir that becomes available if the circumstances require more blood. When the venous circulation makes more blood available, there is a resultant important increase in cardiac output. Thus, the venous circulation, once thought to play a rather passive role in the circulation and serve only as a passageway for the flow of blood, is now recognized as playing an important, active role in the circulation.
It is the function of the capillaries, the thread-like blood vessels that link the arterial with the venous system, to exchange fluid, oxygen, carbon dioxide, nutrients, electrolytes, hormones, and other substances between the blood and the interstitial space, the space outside the capillaries and separating the cells. In the lungs, the capillary system exchanges oxygen and carbon dioxide with the alveoli, the tiny air spaces of the lungs.
Every cell must be in close proximity to a capillary in order to survive. In addition, the capillary walls are very thin, consisting of a single layer of cells, in order to allow the passage of small molecular-sized substances through its wall. There are tiny pores or clefts in the capillary wall which allow passage of molecules from the interior to the exterior of the capillary wall and vice versa. In addition, substances can be transported through the wall with the help of small bubbles, called vesicles, which carry the substance to be transferred within them.
By far, the most important means by which substances are transferred from the plasma, the liquid portion of the blood, and the interstitial fluid surrounding the cells is the process of diffusion. Diffusion allows the passage of substances through the capillary wall without the necessity of pores, clefts or vesicles. Diffusion occurs from an area of high concentration to an area of low concentration. The method of transportation that is used depends on many complex factors including the size of the particle, pressure and concentration differences between the interior and exterior of the capillary, and the solubility of the substance in water and lipids (fats).
The body’s most essential task is the continuous transport of oxygen from the blood to the tissues and the return of oxygen to the blood in exchange for carbon dioxide (CO2). This is the exchange process that occurs in the pulmonary capillary circulation. In the lung, the capillary system takes up oxygen from the alveoli (air sacs) and releases carbon dioxide to be exhaled.
The blood has special carriers for the oxygen it delivers to the tissues; they are the red blood cells, tiny concave discs. Red blood cells are so small that about 75 billion of them would fit into a one-inch cube. Red cells get their color from hemoglobin, a protein that contains iron and is capable of carrying, releasing, and retrieving oxygen.
In the tissues, oxygen leaves the blood for the interstitial fluid by the process of diffusion. The concentration or partial pressure of oxygen in the interstitial fluid is low because it has been used by the cells. On the other hand, the content of oxygen in the capillary is high. Thus, by the process of diffusion, oxygen passes from the area of high concentration to the area of low concentration. Simultaneously, by the same process, carbon dioxide, a waste product of the cells is picked up by the blood and carried by way of the venous circulation to the right atrium and right ventricle and sent to the lungs. The exchange of carbon dioxide for oxygen occurs between the pulmonary capillary system and the alveolus, that tiny air sac in the lungs, which has received oxygen from inhaled air. The process again is one of diffusion across the delicate membrane that separates the pulmonary capillary from the alveolus.
These processes of gas exchange are continuous and essential for survival. Impairment of the process by any mechanism (tissue, lung, or blood) leads to serious consequences. The body does not tolerate continuous low concentrations of oxygen and high concentrations of carbon dioxide for a prolonged period of time.

Anatomy & Physiology of the Heart
Overview of the Cardiovacular System
Hemodynamics of the Cardiac System
The Vascular System